In comments submitted to the Federal Trade Commission (FTC), PhRMA urged the agency to examine how pharmacy benefit managers (PBMs) leverage their extraordinary power to maximize profits, often in ways that harm patients. Our letter urges the FTC to conduct a rigorous analysis to better understand the market power of PBMs, identify conflicts of interest, and address the harms PBMs cause to patients and competition in the health care system.
Here are four key concerns we raised in our comment letter:
1. The influence PBMs have over patient access and affordability of prescription medicines continues to grow. As our letter notes:
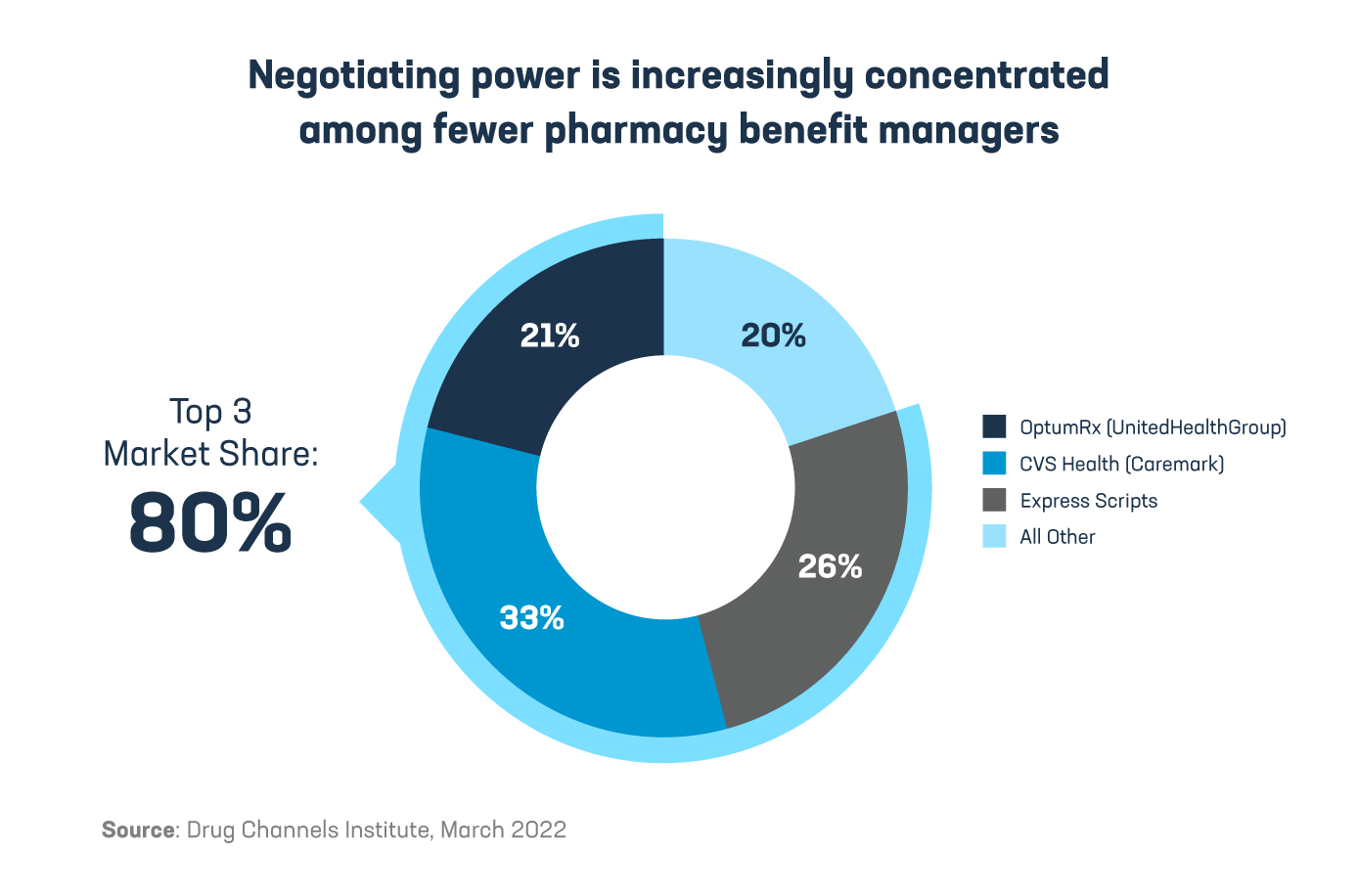
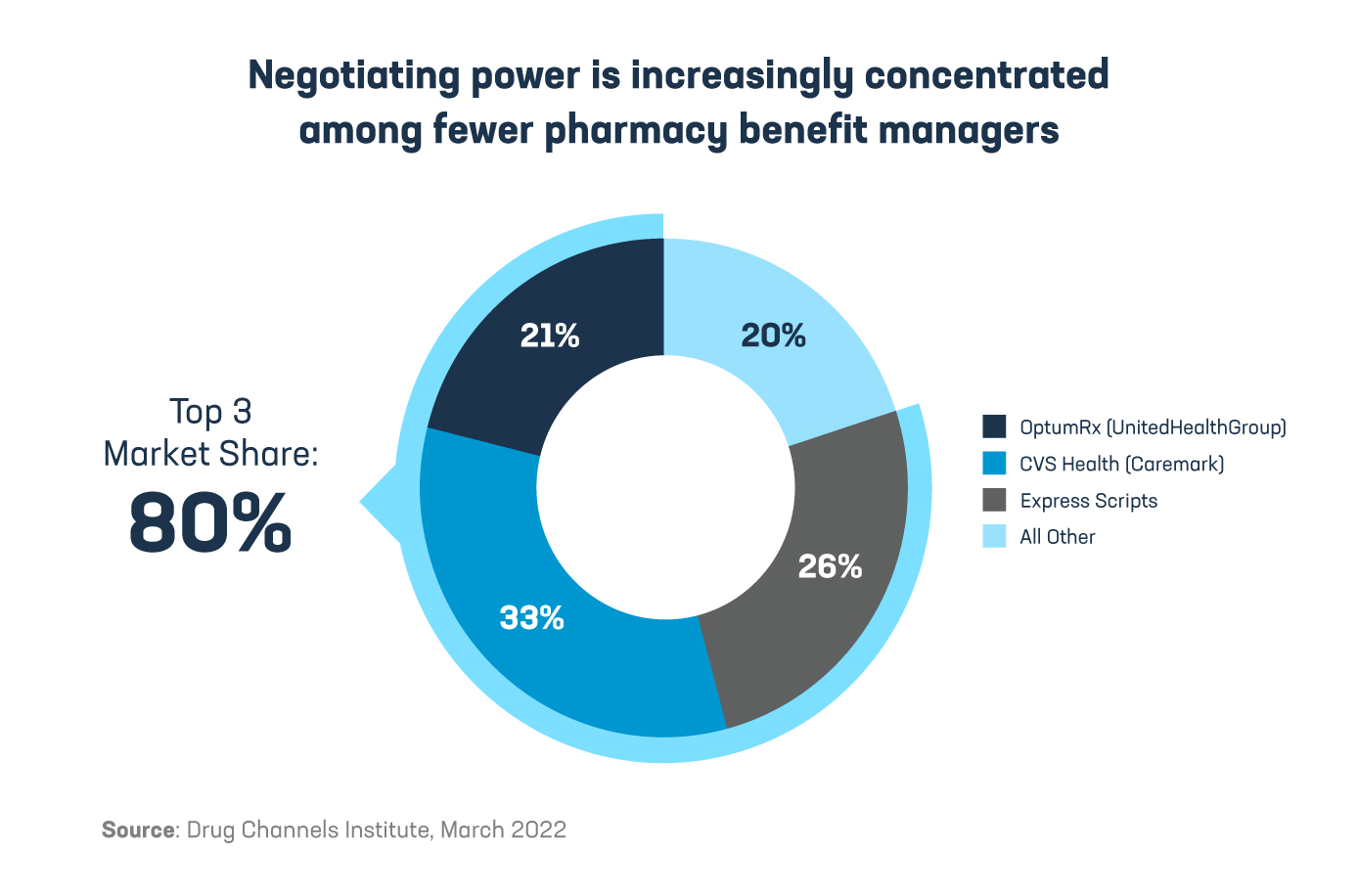
“After nearly two decades of horizontal consolidation, the PBM industry has become increasingly dominated by a small number of large companies… The combined market share of the three largest PBMs has grown significantly, from 48% in 2010 to 80% in 2021.”
“In recent years, the three largest PBMs – CVS Caremark, Express Scripts, and OptumRx – have also combined with health insurers, specialty and mail order pharmacies, and provider groups to form large vertically integrated organizations. These vertically integrated organizations have enormous influence over which medicines patients have access to, the circumstances under which those medicines are covered, when and where they can be dispensed or administered to patients, and the amount paid out of pocket by patients.”
2. PBMs extract large rebates and discounts from manufacturers, but these savings are not always shared with patients. The letter states:
“Negotiating on behalf of health plans, employers, and other payers, PBMs extract billions of dollars from pharmaceutical manufacturers each year… The sheer volume of prescription claims managed by the three largest PBMs provides them with significant leverage in negotiation, often to the detriment of patients and competition.”
“Manufacturer price concessions can significantly lower the net prices of brand medicines, which were 49% lower, on average, than wholesale acquisition costs (i.e., list prices) in 2021.”
“Net prices reflect the final prices paid by PBMs and health plans. Yet in the majority of cases, the net price is not the price available to patients with insurance at the pharmacy counter. Instead, patients with deductibles and coinsurance – who pay a percentage of the cost of their medicine rather than a fixed copayment – are typically required to pay based on the undiscounted list price, rather than the net price that reflects the rebates and discounts paid to the PBM by the manufacturer.”
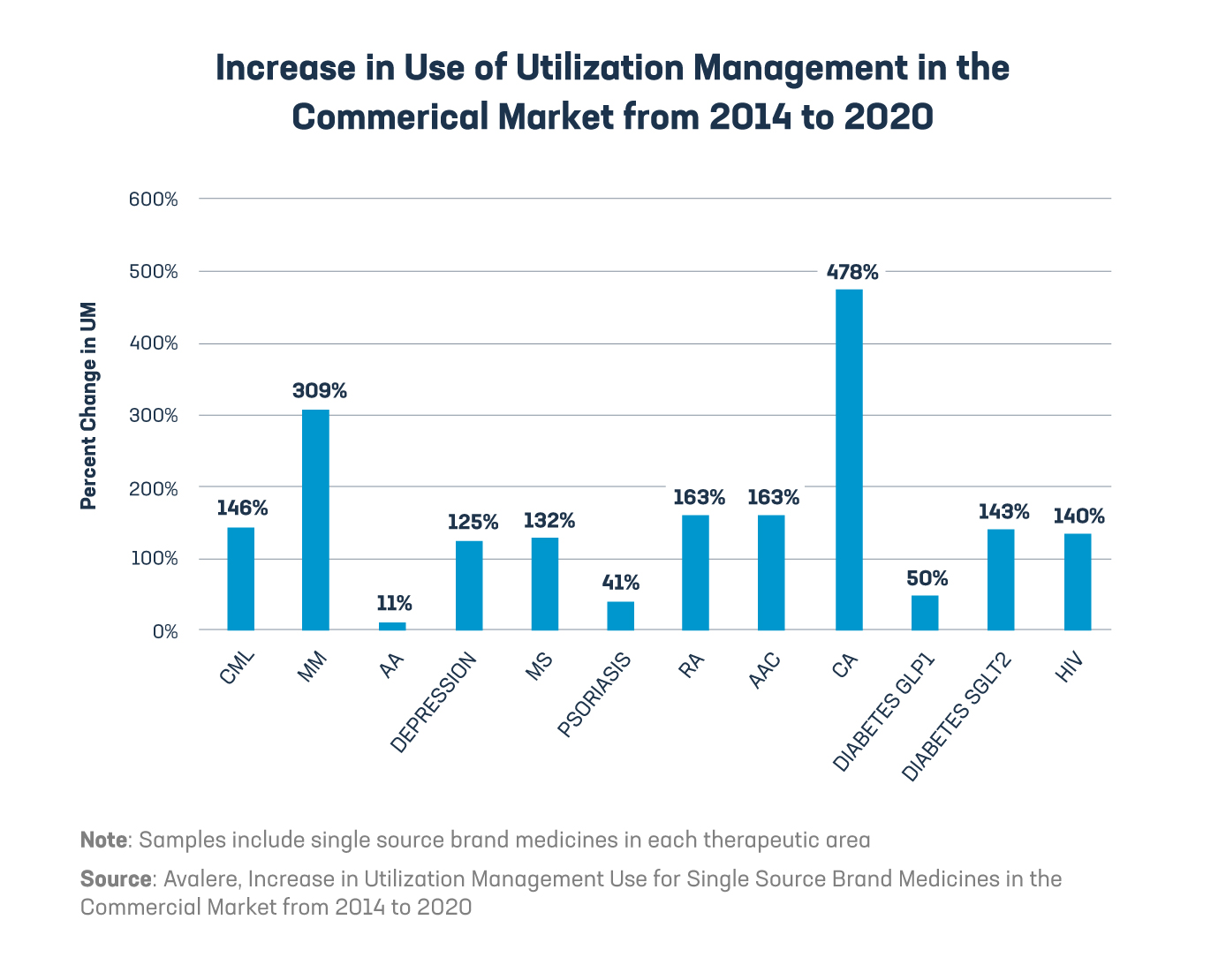
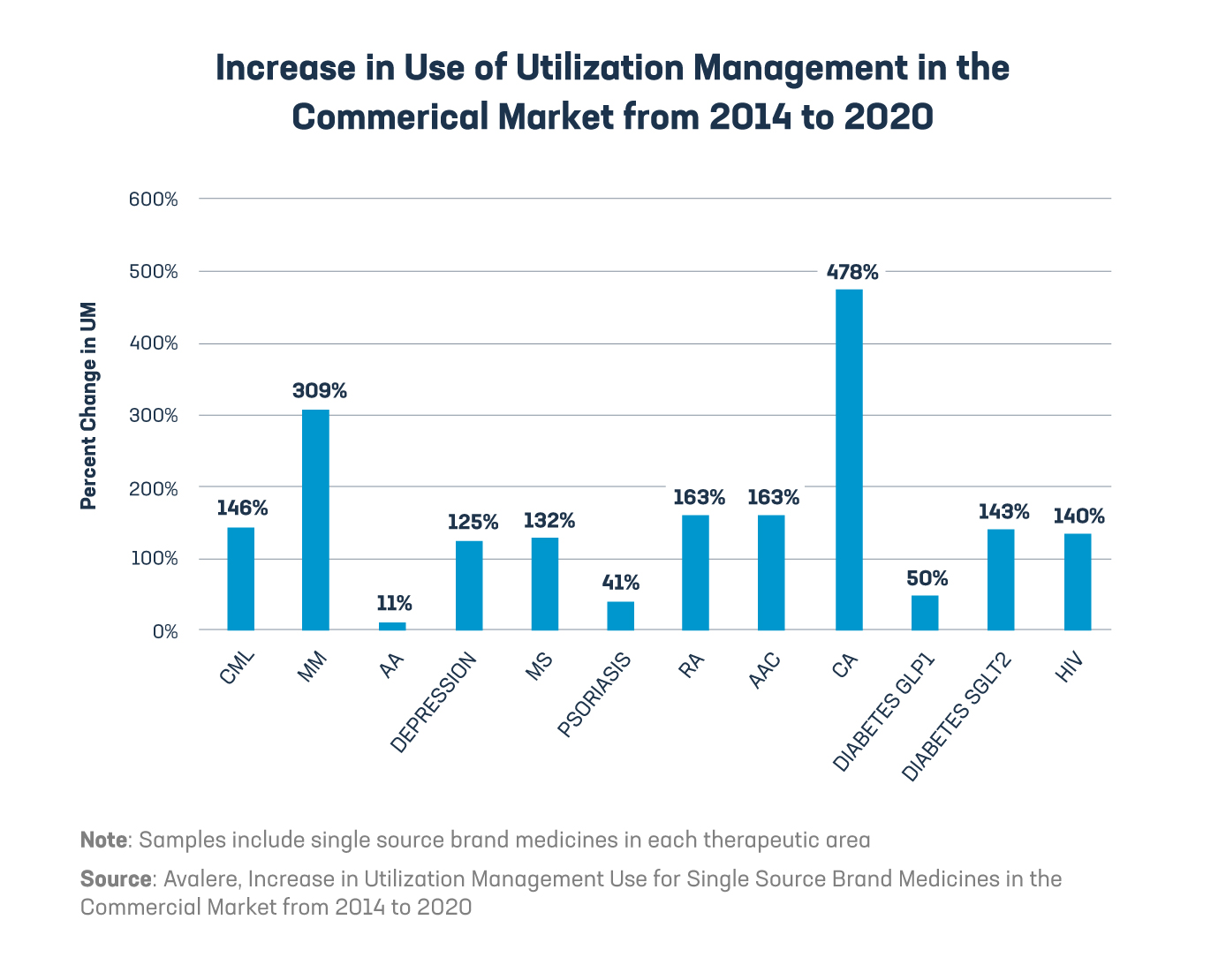
3. PBMs increasingly impose insurance barriers that can limit patient access to medicines. According to our letter:
“The formularies that PBMs establish for their clients govern which medicines are covered, the associated patient cost sharing, and any utilization management or other restrictions on their prescribing or use. PBMs may use a variety of utilization management techniques to direct patients and providers towards their preferred medicines…”
4. A lack of transparency allows PBMs to impose other harmful policies on patients. As the PhRMA letter explains:
“AAPs [accumulator adjustment programs] exclude the value of manufacturer cost-sharing assistance given to eligible commercially insured patients from counting toward patients’ deductibles and out-of-pocket maximums. Copay maximizers adjust individual patient cost sharing upwards to match and exhaust the full value of the manufacturer-provided assistance. PBMs often use these policies to undermine the intended impact of manufacturer cost-sharing assistance programs, which help eligible patients afford their out-of-pocket costs at the pharmacy counter and can significantly improve patient adherence to medicines.”
These and other concerns support our recommendation for the FTC to conduct a rigorous study of the significant role PBMs play in our drug delivery ecosystem and to explore PBM tactics that can result in less access to medicines and higher out-of-pocket costs for patients.
Helping patients means looking at the whole picture, and we are willing to do our part to deliver a stronger, more resilient, affordable and equitable health care system for all patients. The FTC’s review of drug cost middlemen is an important step in the right direction.
Read the full comments here.
Learn more about a better way to lower costs for patients