New data show insurers and middlemen known as pharmacy benefit managers (PBMs) are making it harder for patients to get the medicines they need.
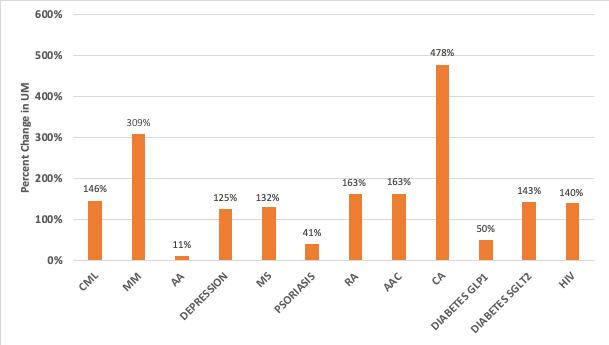
- Patients increasingly face access restrictions to their medicines. Insurers and PBMs use what’s known as utilization management restrictions as a strategy to reduce their spending on medicines, but they can have an adverse impact on patient access. These insurance tactics include prior authorization and fail first requirements (also known as step therapy) and often prevent or delay patients from accessing the medicines they need. A recent analysis by Avalere Health looked at commercial insurers’ use of utilization management for single-source brand medicines across 12 therapeutic areas and found that from 2014 to 2020, these types of restrictions increased across all 12 therapeutic areas, which included cancer, depression, rheumatoid arthritis and diabetes.
Increase in Use of Utilization Management in the Commercial Market from 2014 to 2020
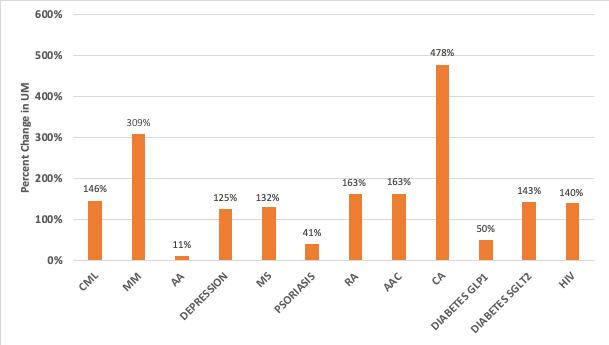
Note: Samples include single-source brand medicines in each therapeutic area
Source: Avalere, Increase in Utilization Management Use for Single-Source Brand Medicines in the Commercial Market from 2014 to 2020
- Fail first requirements are pervasive across commercial health insurance plans. A recent study published in Health Affairs found that a significant share of commercially insured patients taking medicines face step therapy restrictions, where patients must try and fail on one or more medicine preferred by their insurer and PBM before the originally prescribed medicine is covered. In fact, more than half of fail first policies developed by health plans were found to be more restrictive than recommended clinical guidelines, meaning patients and providers may have to overcome time-consuming hurdles before a medicine is covered. The researchers concluded that “[t]hese findings raise questions about potentially overly restrictive step therapy protocols, as well as concerns that variability across health plans makes protocols onerous for patients and practitioners alike.”
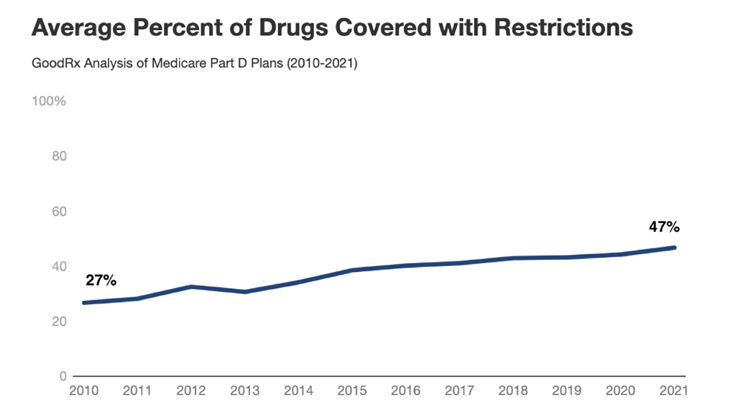
- Access restriction trends in the commercial market also exist in Medicare Part D. A recent report from GoodRx found that the average number of medicines covered by Part D that are subject to utilization management restrictions increased from 27% in 2010 to 47% in 2021. This confirms previous research published by MedPAC that found Medicare beneficiaries now face access barriers for nearly half of all medicines covered in Part D.
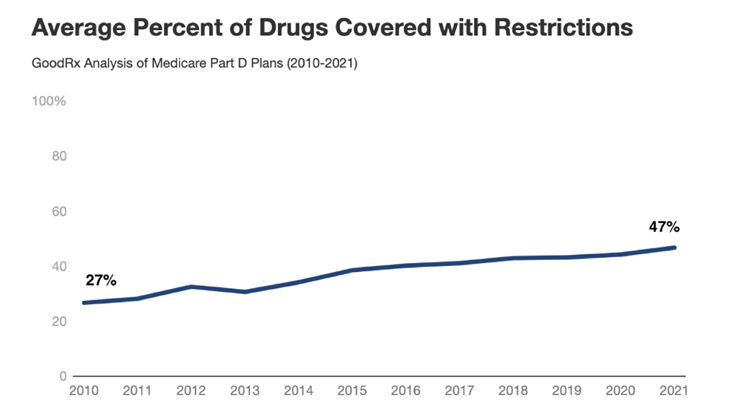
Source: GoodRx, THE BIG PINCH: Findings on Changing Insurance Coverage of Prescription Drugs
These trends are especially concerning considering recent research that shows utilization management restrictions are more likely to affect the sickest and most vulnerable patients in our health care system.
Unfortunately, government price-setting policies currently being considered by Congress threaten to exacerbate these challenges. These policies will ultimately lead to even less access to innovative medicines, while letting health plans and PBMs off the hook for raising costs on patients and restricting access to life-saving treatments.
America’s biopharmaceutical research industry is ready to do its part to help ensure all patients can access the medicines they need. We support patient-centered, bipartisan solutions like making insurance work like insurance by covering more medicines from day one, making out-of-pocket costs more predictable and sharing negotiated savings with patients at the pharmacy counter.
Learn more at PhRMA.org/BetterWay.