3 in 10 insured Americans still face a financial barrier to care and some of the most vulnerable patients are also those more likely to experience barriers in accessing their care, according to our inaugural Patient Experience Survey (PES). This is apparent when we look at the disproportionate application of insurer tools – including prior authorization and failing first – on patients with chronic illnesses and communities of color.
Practices like prior authorization and failing first are designed to keep spending down for insurance companies, but for patients, these practices are roadblocks for receiving the care a patient’s doctor advises, including prescription medicines. If we want to improve health care in this country, insurance must first work like insurance – ensuring patients have access to the medicines and care they need.
Here are three things you should know.
1. Americans face a variety of insurance coverage barriers, like prior authorization and failing first, that can impede access to the medicines they need. 25% of patients report waiting for their insurer to provide prior authorization before accessing a medication their doctor has prescribed. Moreover, one in five Americans report that their insurer required their doctor to prescribe a different medicine than the medicine the doctor believed would be most effective. Doctors should make these decisions, not insurers.
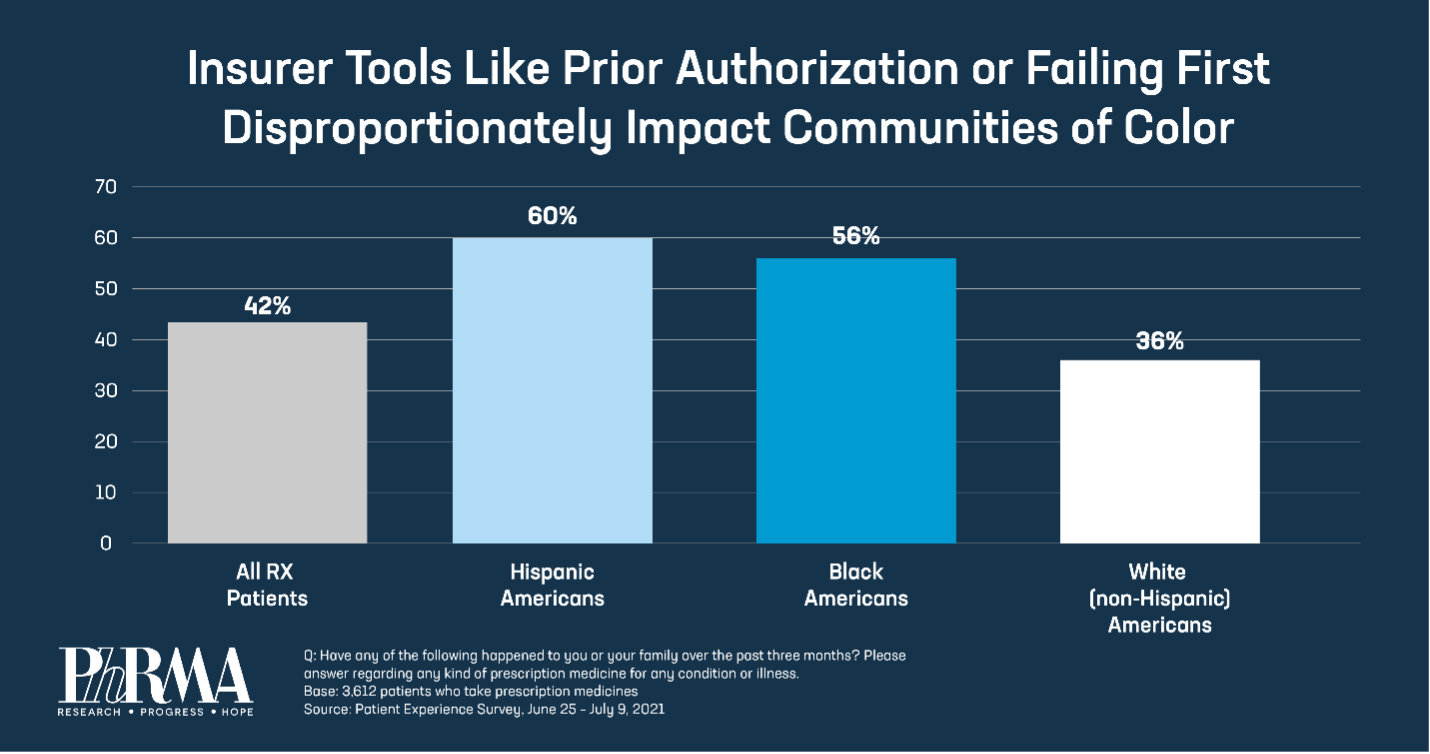
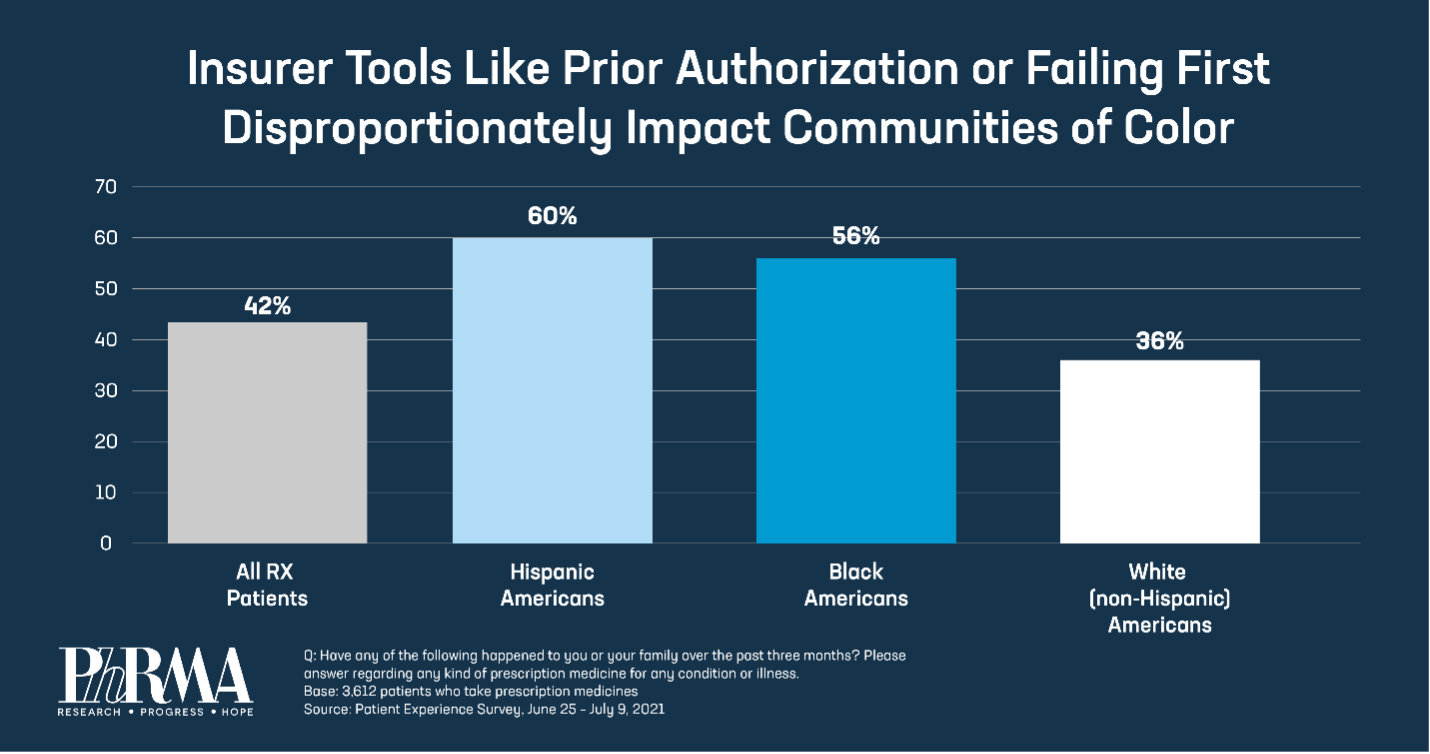
2. Insurance coverage barriers disproportionately impact people with chronic diseases and communities of color. Americans with autoimmune diseases, including allergies (52%) and diabetes (52%), are more likely to report experiences with access barriers, including prior authorization and failing first, than other Americans who take prescription medicines (42%). Additionally, communities of color are significantly more likely to report insurer-imposed barriers: 56% of Black and 60% of Hispanic Americans, compared to 36% of white Americans.
3. Coverage barriers can contribute to patients not taking their medicines as prescribed by a doctor. Of those who were required to undergo step therapy, 57% of these patients also failed to fill or pick up a medicine that had been prescribed. In addition, half of the Americans who reported one or more episodes of non-adherence (not taking their medicines as prescribed) say their health suffered consequently. Moreover, non-adherence increased to 82% for patients with infectious diseases. And those who are unable to take a medicine as prescribed by their doctor often experience worse health outcomes.
For too many Americans, health insurance isn’t providing the level of coverage they need. To resolve systemic health care barriers, we need patient-centered solutions that make insurance work like insurance should by covering more medicines from day one so that patients can access the treatments their doctors prescribe. Read the full Patient Experience Survey here and learn more about our solutions at PhRMA.org/BetterWay.