The second installment of the Patient Experience Survey finds insurer-imposed practices pose significant barriers for Americans as they attempt to access the care they need – and that they are paying for each month in premiums.
Currently, 49% of insured Americans who take prescription medicines report facing barriers such as prior authorization and fail first in the past three months. Prior authorization requires patients to receive approval before their insurer will cover the medicine their doctor prescribed. Step therapy, also known as “fail first,” requires patients to try and fail on one or more medicines before their insurer will cover the medicine originally prescribed. These insurance barriers, among others, not only stand between patients and the medicines they need, but according to our recent findings, are disproportionately imposed on underserved patient populations, including: communities of color and those with mental health conditions. Here are three things you should know:
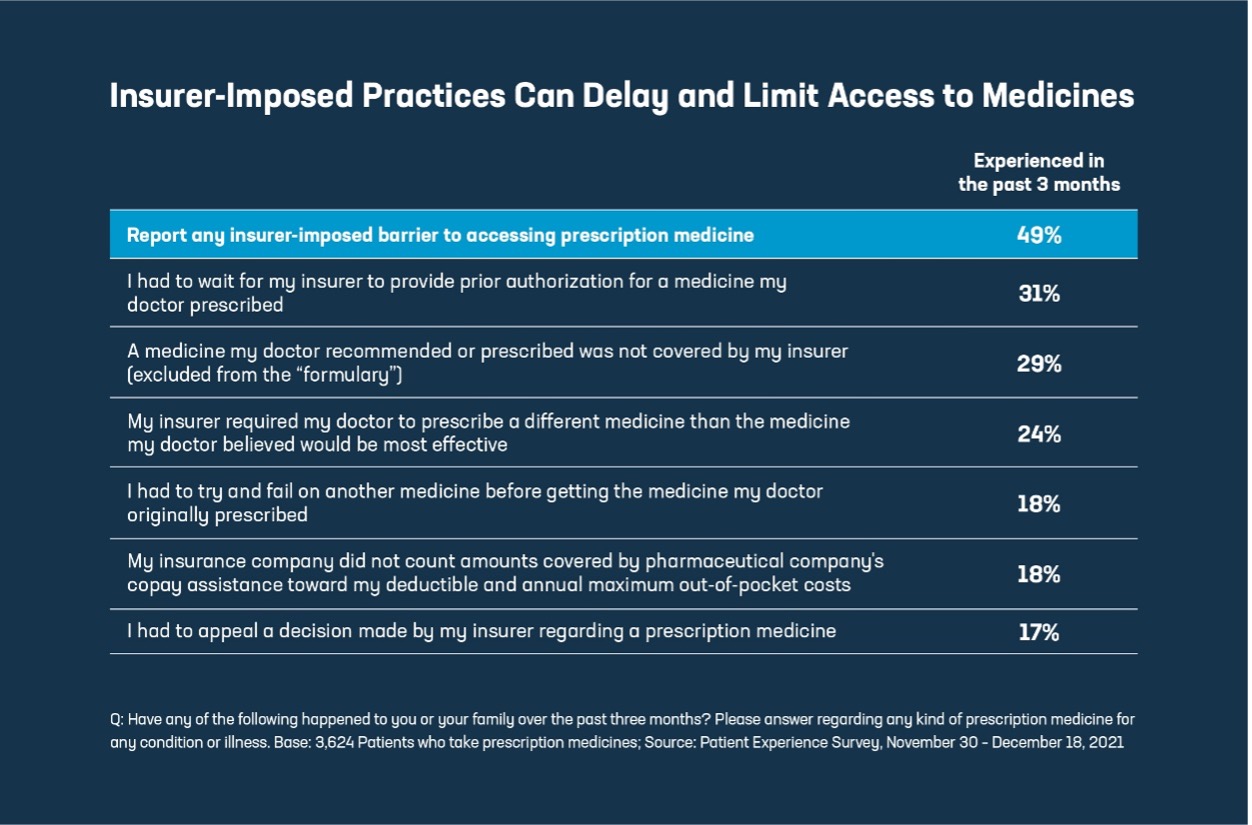
1. Many Americans face insurance barriers when trying to access their medicines. Roughly half (49%) of insured patients who take prescription medicines report facing at least one of these practices (including prior authorization, fail first, exclusion from a formulary, among others) in the past three months, which may have delayed or limited timely access to their medicines.
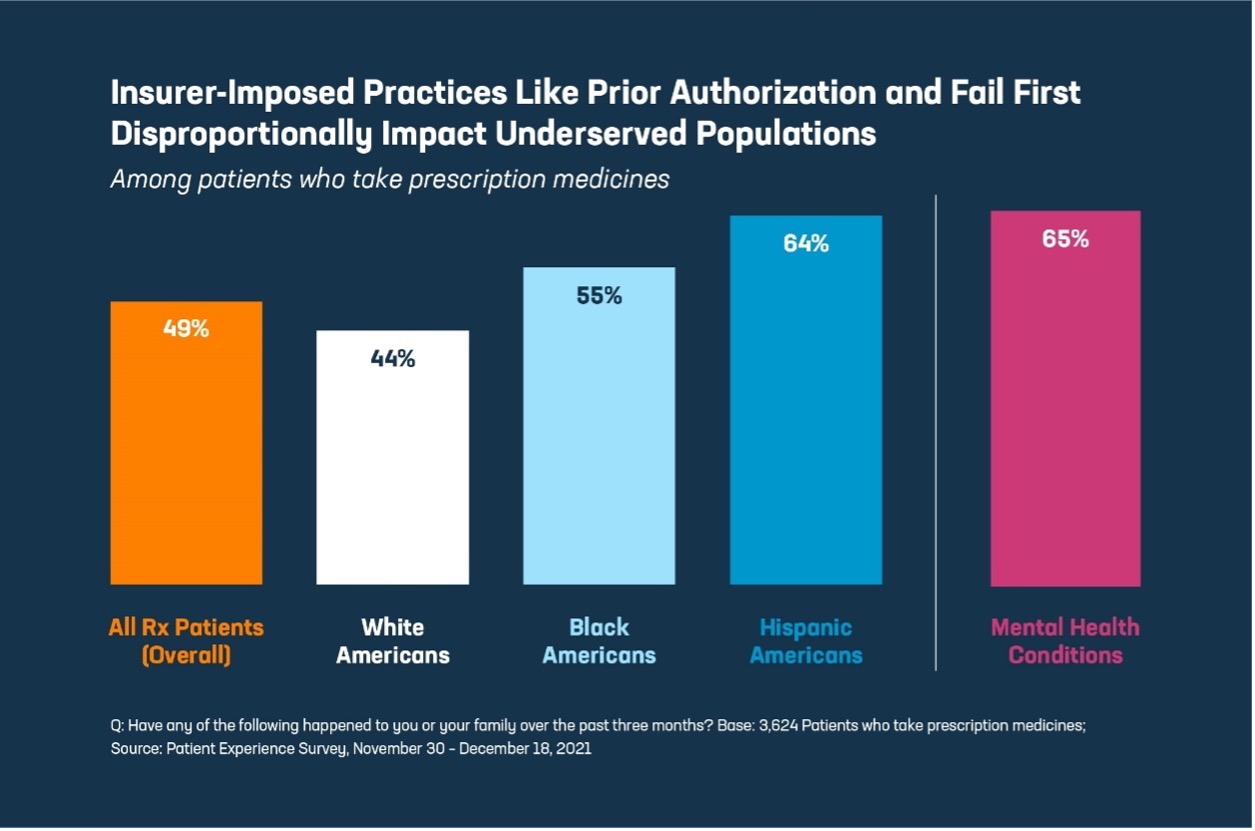
2. The barriers imposed by insurance companies disproportionately affect communities of color and those with mental health conditions. Nearly two thirds (64%) of Hispanic Americans and more than half (55%) of Black Americans who use prescription medicines report experiencing insurance barriers, compared to 44% of white Americans. Patients with mental health conditions also report being disproportionately burdened by access barriers, compared to all Americans using prescription medicines (65% vs. 49%, respectively).
3. Insurer-imposed practices that limit access to prescription medicines can contribute to non-adherence and may lead to poor health outcomes. A patient’s experience with insurance practices like prior authorization and fail first may exacerbate challenges with their health; 75% of patients who reported non-adherence (not taking medicines as prescribed) were subject to at least one insurance barrier. And those unable to take a medicine as prescribed often report worse health outcomes. Almost half (48%) of those reporting medication non-adherence say their health suffered as a result.
For too many Americans, insurance isn’t working like it should. Read more on the patient experience from the first Patient Experience Survey here. To learn more about PhRMA’s patient-centered solutions, visit PhRMA.org/BetterWay.
For topline results, click here.